Eyelid Surgery
Number: 0084
Table Of Contents
PolicyApplicable CPT / HCPCS / ICD-10 Codes
Background
References
Policy
Scope of Policy
This Clinical Policy Bulletin addresses eyelid surgery.
-
Medical Necessity
-
Upper Lid Blepharoplasty:
Upper Lid Blepharoplasty is considered medically necessary for any of the following indications:
- To correct prosthesis difficulties in an anophthalmia socket; or
- To remove excess tissue of the upper eyelid causing functional visual impairment when the following criteria are met:
- PhotographsFootnote1* taken within the past 12 months in straight gaze show redundant eyelid tissue overhanging the upper eyelid margin or resting on or pushing down on the eye lashes; and
- Documentation of visual field testingFootnote2** within the past 12 months, performed with and without the eyelid or brow taped, showing both of the following:
- A superior visual field of 30 degrees or less prior to taping; and
- Either of the following after taping of the eyelids:
- an increase in superior visual fields of 12 degrees or more; or
- a 30 percent or greater increase in superior visual fields; or
- PhotographsFootnote1* taken within the past 12 months in straight gaze show redundant eyelid tissue overhanging the upper eyelid margin or resting on or pushing down on the eye lashes; and
- To relieve painful symptoms of blepharospasm; or
- To treat peri-orbital sequelae of thyroid disease and nerve palsy, and peri-orbital sequelae of other nerve palsy (e.g., the oculomotor nerve).
Note: For members with unilateral disease meeting criteria for the above-listed procedures, surgery of the contralateral eye may be considered medically necessary to obtain symmetry.
-
Lower Lid Blepharoplasty:
Lower Lid Blepharoplasty is considered medically necessary for any of the following indications
- To correct prosthesis difficulties in an anophthalmia socket; or
- To relieve excessive lower lid bulk only if proper positioning of prescription eyeglasses is precluded and is secondary to conditions such as:
- Chronic systemic corticosteroid therapy;; or
- Dermatomyositis; or
- Graves’ disease; or
- Myxedema; or
- Nephrotic syndrome; or
- Polymyositis; or
- Scleroderma; or
- Sjögren’s syndrome; or
- Systemic lupus erythematosus.
Notes: For members with unilateral disease meeting criteria for the above-listed procedures, surgery of the contralateral eye may be considered medically necessary to obtain symmetry.
Excess tissue beneath the eye rarely obstructs vision, so the lower lid blepharoplasty is rarely considered medically necessary for functional visual impairment.
-
Upper Lid Ptosis Surgery:
Ptosis (blepharoptosis) repair for laxity of the muscles of the upper eyelid causing functional visual impairment when the following criteria are met:
- PhotographsFootnote1* taken within the past 12 months of the individual looking straight ahead demonstrating the eyelid at or below the upper edge of the pupil; and
- Documentation of visual field testingFootnote2** within the past 12 months, performed with and without the eyelid or brow taped, showing both of the following:
- A superior visual field of 30 degrees or less prior to taping; and
- Either of the following after taping of the eyelids:
- an increase in superior visual fields of 12 degrees or more; or
- a 30 percent or greater increase in superior visual fields; and
-
Documentation in the medical records of the margin reflex differenceFootnote3*** (distance from the upper lid margin to the reflected corneal light reflex at normal gaze) of 2 mm or less with the eyes in a straight gaze.
Note: For members with unilateral disease meeting criteria for the above-listed procedures, surgery of the contralateral eye may be considered medically necessary to obtain symmetry.
-
Brow Ptosis Surgery:
Brow ptosis repair for laxity of the forehead muscles causing functional visual impairment is considered medically necessary when the following criteria are met:
- PhotographsFootnote1* taken within the past 12 months show the eyebrow below the supra-orbital rim; and
- Documentation of visual field testingFootnote2** within the past 12 months, performed with and without the eyelid or brow taped, showing both of the following:
- A superior visual field of 30 degrees or less prior to taping; and
- Either of the following after taping of the eyelids:
- an increase in superior visual fields of 12 degrees or more; or
- a 30 percent or greater increase in superior visual fields; and
-
Brow ptosis is causing a functional impairment of upper/outer visual fields with documented interference with vision or visual field related activities such as difficulty reading due to upper eyelid drooping, looking through the eyelashes or seeing the upper eyelid skin.
Note: For members with unilateral disease meeting criteria for the above-listed procedures, surgery of the contralateral eye may be considered medically necessary to obtain symmetry.
-
Ectropion / Entropion Repair
Eyelid ectropion or entropion repair is considered medically necessary to repair defects predisposing to corneal or conjunctival injury due to ectropion (eyelid turned outward), entropion (eyelid turned inward), or pseudotrichiasis (inward direction of eyelashes due to entropion) when selection criteria are met.
-
Selection Criteria for Ectropion
Clear high-quality, clinical photographsFootnote1* must document the presence of an ectropion, and corneal or conjunctival injury with both of the following:
- Subjective symptoms including either excess tearing, or pain/discomfort; and
- Any one of the following:
- Corneal ulcer
- Exposure keratitis
- Kerato-conjunctivitis
-
Selection Criteria for Entropion
Clear high-quality, clinical photographsFootnote1* must document:
Lid turned inward; and at least one of the following:
- Trichiasis or irritation of cornea or conjunctiva; or
- Subjective symptoms including either excessive tearing, or pain/discomfort.
Note: For members with unilateral disease meeting criteria for the above-listed procedures, surgery of the contralateral eye may be considered medically necessary to obtain symmetry.
-
-
Upper Eyelid Tightening Procedures:
Block resection or tarsal strip with lateral canthal tightening are considered medically necessary for members who have:
- Refractory corneal; or
- Conjunctival inflammation related to exposure from floppy eyelid syndrome.
Note: For members with unilateral disease meeting criteria for the above-listed procedures, surgery of the contralateral eye may be considered medically necessary to obtain symmetry.
Footnote1* Note: Where medical necessity criteria indicate need for photographs, photos must be taken with the eyes not dilated or squinting. Photos are to be taken at eye level and depicting a frontal view. Photos must be of sufficient quality to show the light reflex on the cornea, and demonstrate the lid margins in relation to the pupil.Excess upper eyelid skin, upper eyelid ptosis, or brow ptosis can be present alone or in any combination, and each may require correction. If both a blepharoplasty and ptosis repair are requested, 2 photographs may be necessary to demonstrate the need for both procedures: 1 photograph should show the excess skin above the eye resting on the eyelashes, and a second photograph should show persistence of lid lag, with the upper eyelid crossing or slightly above the pupil margin, despite lifting the excess skin above the eye off of the eyelids with tape. If all 3 procedures (i.e., blepharoplasty, blepharoptosis repair, and brow ptosis repair) are requested, 3 photographs may be necessary.
Footnote2** Note: A normal, unobstructed superior visual field measures approximately 45 to 50 degrees. A superior visual field of 30 degrees or less corresponds to a functional superior visual field loss. Surgery is indicated for persons with a superior visual field of 30 degrees or less if there is an increase of 12 degrees or more, or a 30 percent or greater increase, in superior visual fields after taping of the eyelids. This is illustrated by the following examples:
Example A: A visual field of 25 degrees that increases to 37 degrees after taping would meet visual field criteria for surgery.
Example B: A visual field of 30 degrees that increases to 39 degrees after taping would meet visual field criteria for surgery.
Visual field testing should be performed within the past 12 months. Visual field testing may be completely automated (such as Humphrey Visual Field), or performed by a technician with or without the assistance of a machine (such as Goldmann Perimetry). Both taped and untaped visual fields need to be submitted for each eye for requested surgery.
Footnote3*** Note: A margin to reflex distance (MRD) of 2 mm corresponds to a superior visual field impairment of 12-15 degrees. Thus, a baseline superior visual field of 30-35 degrees corresponds to an MRD of 2 mm.
-
Congenital Ptosis Surgery:
Aetna considers surgical correction of congenital ptosis medically necessary to allow proper visual development in infants and children when the following criteria are met:
- Infant or child has congenital ptosis (present at birth and detected within the first year of life); and
- Ptosis interferes with field of vision (visual field testing not required); and
- Child has abnormal head posture (e.g., head tilt or turn, chin up or chin down), amblyopia or strabismus.
-
-
Experimental and Investigational
Periorbital Microcystic Lymphatic Malformation with Blepharoptosis:
Aetna considers intralesional bleomycin injection experimental and investigational for the treatment of periorbital microcystic lymphatic malformation with blepharoptosis because its effectiveness has not been established.
-
Cosmetic
Congenital Ptosis:
Surgery is considered cosmetic if performed for mild ptosis that is only of cosmetic concern.
-
Related CMS Coverage Guidance
This Clinical Policy Bulletin (CPB) supplements but does not replace, modify, or supersede existing Medicare Regulations or applicable National Coverage Determinations (NCDs) or Local Coverage Determinations (LCDs). The supplemental medical necessity criteria in this CPB further define those indications for services that are proven safe and effective where those indications are not fully established in applicable NCDs and LCDs. These supplemental medical necessity criteria are based upon evidence-based guidelines and clinical studies in the peer-reviewed published medical literature. The background section of this CPB includes an explanation of the rationale that supports adoption of the medical necessity criteria and a summary of evidence that was considered during the development of the CPB; the reference section includes a list of the sources of such evidence. While there is a possible risk of reduced or delayed care with any coverage criteria, Aetna believes that the benefits of these criteria – ensuring patients receive services that are appropriate, safe, and effective – substantially outweigh any clinical harms.
Code of Federal Regulations (CFR):
42 CFR 417; 42 CFR 422; 42 CFR 423.
Internet-Only Manual (IOM) Citations:
CMS IOM Publication 100-02, Medicare Benefit Policy Manual; CMS IOM Publication 100-03 Medicare National Coverage Determination Manual.
Medicare Coverage Determinations:
Centers for Medicare & Medicaid Services (CMS), Medicare Coverage Database [Internet]. Baltimore, MD: CMS; updated periodically. Available at: Medicare Coverage Center. Accessed November 7, 2023.
-
Related Policies
| Code | Code Description |
|---|---|
Information in the [brackets] below has been added for clarification purposes. Codes requiring a 7th character are represented by "+": |
|
Blepharoplasty: |
|
CPT codes covered if selection criteria are met: |
|
| 15820 | Blepharoplasty, lower eyelid |
| 15821 | with extensive herniated fat pad [excess tissue beneath the eye rarely obstructs vision so lower lid blepharoplasty is rarely covered for this indication] |
| 15822 | Blepharoplasty, upper eyelid |
| 15823 | with excessive skin weighing down lid |
Other CPT codes related to the CPB: |
|
| 21280 | Medial canthopexy |
| 21282 | Lateral canthopexy |
| 61330 | Decompression of orbit only, transcranial approach |
| 67414 | Orbitotomy without bone flap (frontal or transconjunctival approach); with removal of bone for decompression |
| 67445 | Orbitotomy with bone flap or window, lateral approach (e.g., Kroenlein); with removal of bone for decompression |
| 67950 | Canthoplasty (reconstruction of canthus) |
ICD-10 codes covered if selection criteria are met: |
|
| C44.101 - C44.1992 | Other and unspecified malignant neoplasm of skin of eyelid, including canthus |
| D21.0 | Benign neoplasm of connective and other soft tissue of head, face and neck [Medial or lateral canthus] |
| H02.001 - H02.059 | Entropion and trichiasis of eyelid |
| H02.831 | Dermatochalasis of right upper eyelid |
| H02.834 | Dermatochalasis of left upper eyelid |
| H04.201 - H04.219 | Epiphora unspecified as to cause and due to excess lacrimation |
| H05.89 | Other disorders of orbit [Endocrine exophthalmos] |
| Z85.828 | Personal history of other malignant neoplasm of skin [medial or lateral canthus] |
| Z86.018 | Personal history of other benign neoplasm [medial or lateral canthus] |
Ptosis repair: |
|
CPT codes covered if selection criteria are met: |
|
| 67900 | Repair of brow ptosis (supraciliary, mid-forehead or coronal approach) |
| 67901 | Repair of blepharoptosis; frontalis muscle technique with suture or other material (e.g., banked fascia) |
| 67902 | frontalis muscle technique with autologous fascial sling (includes obtaining fascia) |
| 67903 | (tarso) levator resection or advancement, internal approach |
| 67904 | (tarso) levator resection or advancement, external approach |
| 67906 | superior rectus technique with fascial sling (includes obtaining fascia) |
| 67908 | conjunctivo-tarso-Muller's muscle-levator resection (e.g., Fasanella-Servat type) |
| 67909 | Reduction of overcorrection of ptosis |
Other CPT codes related to the CPB: |
|
| 11900 - 11901 | Injection, intralesional |
| 92081 - 92083 | Visual field examination [not routinely necessary for excess upper eyelid skin, upper eyelid ptosis, or brow ptosis] |
ICD-10 codes covered if selection criteria are met: |
|
| H02.401 - H02.439 | Ptosis of eyelid [causing functional visual impairment] |
| Q10.0 | Congenital ptosis [moderate to severe] |
Intralesional bleomycin injection: |
|
HCPCS codes not covered for indications listed in the CPB: |
|
| J9040 | Injection, bleomycin sulfate, 15 units |
ICD-10 codes not covered for indications listed in the CPB: |
|
| I89.9 | Other specified noninfective disorders of lymphatic vessels and lymph nodes [peri-orbital microcystic lymphatic malformation with blepharoptosis] |
| Q15.8 | Other specified congenital malformations of eye [peri-orbital microcystic lymphatic malformation with blepharoptosis] |
Ectropion repair: |
|
CPT codes covered if selection criteria are met: |
|
| 67914 | Repair of ectropion; suture |
| 67915 | thermocauterization |
| 67916 | excision tarsal wedge |
| 67917 | extensive (eg, tarsal strip operations) |
ICD-10 codes covered if selection criteria are met: |
|
| H02.101- H02.139 | Ectropion of eyelid |
| H02.151 - H02.159 | Paralytic ectropion |
| Q10.1 | Congenital ectropion |
Entropion repair: |
|
CPT codes covered if selection criteria are met: |
|
| 67921 | Repair of entropion; suture |
| 67922 | thermocauterization |
| 67923 | excision tarsal wedge |
| 67924 | extensive (eg, tarsal strip or capsulopalpebral fascia repairs operation) |
ICD-10 codes covered if selection criteria are met:: |
|
| H02.001 - H02.039 | Entropion of eyelid |
| Q10.2 | Congenital entropion |
Background
Blepharoplasty refers to surgery to remove excess skin and fatty tissue around the eyes. Blepharochalasis is a term used to refer to loose or baggy skin (dermatochalasis) above the eyes, so that a fold of skin hangs down, often concealing the tarsal margin when the eye is open. In severe cases, excess skin and fat above the eyes can sit on the upper eyelid and may obstruct the superior field of vision. Blepharochalasis may cause pseudoptosis (false ptosis), where the patient has a normal ability to elevate the eyelid, but bagging skin above the eye overhangs the eyelid margin, resembling ptosis. In some cases, excess skin around the eye may cause the eyelashes to turn in and to irritate the eye, or turn outward, resulting in exposure keratitis.
Surgical removal of these overhanging skin folds may improve the function of the upper eyelid and restore peripheral vision. Blepharoplasty is also performed for cosmetic reasons to improve a sagging, tired appearance, and is the second most common aesthetic procedure performed by plastic surgeons. For coverage of this procedure, photographs in straight gaze should show sagging tissue above the eyes that is resting on or pushing down on the eyelashes.
Blepharoplasty to remove excess tissue either above or below the eyes may also be medically necessary and covered to correct prosthesis difficulties in an anophthalmia socket, to repair defects caused by trauma or tumor-ablative surgery, to correct an entropion (inward turned eyelid) or ectropion (outward turned eyelid), to treat peri-orbital sequelae of thyroid disease and nerve palsy, and to relieve painful blepharospasm.
Ptosis (also called blepharoptosis) is the term for drooping of one or both upper eyelids. This may occur in varying degrees from slight drooping to complete closure of the involved eyelid. In the most severe cases, the drooping can obstruct the visual field and cause positional head changes. There are 2 types of ptosis:- acquired and
- congenital.
Acquired ptosis is more common. Congenital ptosis is present at birth. Ptosis may occur because the levator muscle's attachment to the lid is weakening with age. Acquired ptosis can also be caused by a number of different things, such as disease that impairs the nerves, diabetes, injury, tumors, inflammation, or aneurysms. Congenital ptosis may be caused by a problem with nerve innervation or a weak muscle. Drooping eyelids may also be the result of diseases such as myotonic dystrophy or myasthenia gravis. The primary symptom of ptosis is a drooping eyelid. Adults will notice a loss of visual field because the upper portion of the eye is covered. Children who are born with a ptosis usually tilt their head back in an effort to see under the obstruction. Some people raise their eyebrows in order to lift the lid slightly and therefore may appear to be frowning.
Diagnosis of ptosis is usually made by observing the drooping eyelid. Ptosis is usually treated surgically. Surgery can generally be done on an outpatient basis under local anesthetic. For minor drooping, a small amount of the eyelid tissue can be removed. For more pronounced ptosis the approach is to surgically shorten the levator muscle or connect the lid to the muscles of the eyebrow. Or, the aponeurosis can be re-attached to the tarsal plate if it had separated. Correcting the ptosis is usually done only after determining the cause of the condition.
Ptosis (blepharoptosis) repair for laxity of the muscles of the upper eyelid causing functional visual impairment is covered when photographs in straight gaze show the eyelid margin across the midline or at the most 1 or 2 mm above the midline of the pupil (see Figure).
Figure: Diagram of upper lid margin crossing the pupil
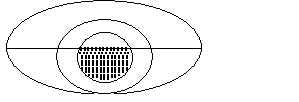
To demonstrate the medical necessity of both blepharoplasty and ptosis (blepharoptosis) repair, 2 sets of photographs may be needed. One set of photographs (front and side views) should demonstrate the excess skin above the eyes resting on the eyelashes. A second set of photographs should be taken with the excess skin lifted off of the eyelashes (such as by taping the excess skin to the forehead), and demonstrating persistence of ptosis with the lid margin across the midline of the pupil or 1 to 2 mm above the pupil midline.
Brow ptosis refers to sagging tissue of the eyebrows and/or forehead. In extreme cases, brow ptosis can obstruct the field of vision. Brow ptosis is caused by aging changes in the forehead muscle and skin, which leads to weakening of these tissues and sagging of the eyebrows. Brow ptosis is treated surgically with the specific operation being based on the amount and location of the brow ptosis.
Brow ptosis surgery is usually performed under local anesthesia as an outpatient procedure. Excess skin and muscle is excised and the deep tissues are sutured together. Brow ptosis repair for laxity of the forehead muscles causing functional visual impairment is covered when photographs show the eyebrow below the supra-orbital rim.
Often brow ptosis coexists with eyelid ptosis and dermatochalasis; in these cases, ptosis surgery and blepharoplasty may be performed at the time of the brow ptosis surgery. The medical necessity of each surgical procedure may need to be demonstrated with separate photographs: 1 photograph should show the eyebrow below the supra-orbital rim, a second photograph with the sagging forehead lifted up in order to see the sagging tissue above the eye resting on the eyelashes, and then a third with the sagging tissue lifted off of the eyelid in order to see the persistent lid lag (ptosis).
Canthoplasty, also known as inferior retinacular suspension or lateral retinacular suspension, involves tightening the muscles or ligaments that provide support to the outer corner of the eyelid. This procedure may be medically necessary where drooping of the outer corner of the eyelid interferes with vision.
Visual field testing measures the entire scope of vision by creating an individual "map" of each eye. With one eye covered, the individual responds to light and/or various intensities of movement by pushing a button, allowing the computer to generate a map of the visual fields. Testing may be completely automated or performed by a technician with or without the assistance of a machine. Testing the central 24 degrees or 30 percent of the visual field is most commonly used.
Visual field testing alone is not sufficient to determine the presence of excess upper eyelid skin, upper eyelid ptosis, or brow ptosis. A patient could cause a visual field defect by lowering their lids during the test. Photographs that document eyelids crossing the pupils provide additional support for the need of surgery.
If visual field tests are performed, the tests should show loss of 2/3 or greater of a visual field in the upper or temporal areas documented by computerized visual field studies, with visual field restored by taping or holding up the upper lid.
An UpToDate review on ptosis (Lee, 2013) states that "In patients with third nerve [oculomotor nerve] palsy, an interval of 6 to 12 months before surgical intervention is advised because many will have spontaneous recovery. Similarly, patients with MG [myasthenia gravis] should have stable disabling ptosis for several months on maximal medical therapy before considering surgical therapy".
Hollander and associates (2019) noted that various functional outcomes after upper blepharoplasty have been reported in the literature. In a systematica review, these investigators examined the literature to evaluate the objective and subjective functional effects of upper blepharoplasty. After a systematic search of 4 search engines (PubMed, Embase, Cinahl and Cochrane), any study on objective and subjective (patient reported) functional outcome after upper blepharoplasty was subjected to a quality assessment for possible inclusion in the review. The intervention was defined as a solitary surgical upper blepharoplasty containing the removal of skin, with or without the removal of a strip of orbicularis oculi muscle and/or upper orbital fat. Eligible studies were randomized controlled trials (RCTs), controlled trials, cohort studies and case series (n of greater than or equal to 10). A total of 3,525 studies were assessed, of which 28 studies were included in this systematic review. Favorable outcomes after an upper blepharoplasty were reported and included enlarged visual field, enhanced quality of life (QOL) related to fewer headaches and improved vision. Furthermore, sensitivity of the eyelids decreased, with differences in recovery. Outcomes for eyebrow height, astigmatism, contrast sensitivity and eyelid kinematics were not consistent between the studies. No meta-analysis could be performed due to the limited scope of included studies and the great variety in outcomes and blepharoplasty techniques. The authors concluded that upper blepharoplasty was accompanied by a great variety of beneficial functional outcomes including an increased visual field and improvement in headache- and vision-related QOL. Moreover, these researchers stated that further research is needed, especially where results were conflicting (effects on eye dryness and eyebrow height) and/or the data were limited (contrast sensitivity, astigmatism).
Hollander and colleagues (2020) stated that although upper blepharoplasty is a common cosmetic surgical intervention, a better scientific understanding of the aesthetic results and the preferred surgical technique to achieve the best aesthetic results is still needed. These investigators carried out a systematic search using 4 search engines (PubMed, Embase, CINAHL, and Cochrane) to identify any study on the aesthetic outcome of a solitary upper blepharoplasty; these were subjected to quality assessment for possible inclusion. Eligible studies were RCTs, controlled studies, cohort studies, and case series (n of greater than or equal to 10). A total of 4,043 studies were examined, of which 26 were included. Aesthetic outcomes included patient-reported outcome measures, scarring, eyebrow height, tarsal platform show, and panel or expert evaluation; meta-analysis was not possible. Patients were generally satisfied with the aesthetic result and scar formation after an upper blepharoplasty. The amount of tarsal platform showed increases, which positively affected the aesthetics. The eyebrow appeared to move down slightly. The surgical technique used (skin only or skin/muscle removal) did not influence patient satisfaction or the physician-assessed aesthetic outcomes. Patients were generally satisfied after an upper blepharoplasty. The authors concluded that the optimal design of the skin excision is still a matter of debate, especially when addressing lateral hooding; further objective research is advised.
Botulinum Toxin Type A (Botox)-Induced Ptosis
King (2016) noted that in aesthetic medicine, ptosis is almost exclusively related to the inadvertent injection of botulinum toxin type A (Botox) into an unwanted area leading to muscle weakness and a resultant droop, especially in the hands of an inexperienced injector. Depending on the area treated, ptosis can affect the brow resulting in a lowering of the eyebrows, which produces a poor cosmetic result but can also lead to a significant descent of the eyebrows that may interfere with vision. Upper lid ptosis may occur when treating the glabellar complex and Botox diffuses through the orbital septum and affects the lid elevator muscle either as it traverses the pre-periosteal plane, or the toxin may track along tributaries of the superior ophthalmic vein. This may result in a drooping of the upper lid with the patient unable to fully open the eye, a poor cosmetic result that may interfere with normal vision.
For individuals being considered for ptosis repair surgery, they should not have had botulinum toxin type A (Botox) injection in the forehead in past 6 months.
Intralesional Bleomycin Injection
Yang et al (2015) stated that peri-orbital microcystic lymphatic malformations (LM) can cause severe symptoms, such as blepharoptosis, amblyopia, chemosis, strabismus, diminished vision, and blindness. In a retrospective study, these researchers evaluated the clinical outcome in peri-orbital microcystic LM patients with blepharoptosis who underwent surgical treatment combined with intralesional bleomycin injection. A total of 9 patients diagnosed as peri-orbital microcystic LM with blepharoptosis were included in this study. All of them underwent surgical treatment and bleomycin injection from January 2010 to January 2014. The lesion was resected through the lower eyebrow and/or a coronal incision at the first stage, and levator resection was performed at the second stage. Any persistent lesion or its recurrence was managed by intralesional bleomycin injection. Blepharoptosis and visual obstruction were corrected in all patients. Mean follow-up was 24.6 months; 6 patients had recurrence during follow-up; and 2 patients who had partial eyelid closure after the second stage surgery recovered in 3 months. Amblyopia, astigmatism, and strabismus were not improved after treatment. All patients had excellent aesthetic improvement and corrected blepharoptosis. The authors concluded that resection through a lower eyebrow and coronal incision and levator resection performed in 2 stages can quickly correct the visual impairment caused by peri-orbital microcystic LM with blepharoptosis. They stated that intralesional bleomycin injection is a promising adjunctive therapy for residual or recurrent lesions after surgery.
Eyelid Surgery for Upper Visual Field Improvement
On behalf of the American Society of Plastic Surgeons, a group of experts from different disciplines was convened to develop guidelines for the management of upper visual field impairments related to eyelid ptosis and dermatochalasis (Kim et al, 2022). The objective was to provide evidence-based recommendations to improve patient care. A multi-disciplinary group of experts representing their specialty organizations was selected. They carried out a systematic review including topics regarding documentation of the underlying cause for visual field impairment, selection of an appropriate surgical repair, assessment of the type of anesthesia, the use of adjunctive brow procedures, and follow-up assessments. The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology process was employed to examine the relevant studies. Clinical practice recommendations were developed using BRIDGE-Wiz (Building Recommendations In a Developers' Guideline Editor) software. Each topic area was assessed. A clinical recommendation was made, and the relevant literature was discussed. The authors concluded that the review of the literature revealed varied complication rates and diverse treatment modalities for the correction of upper visual field deficit. Strong recommendations could not be rendered in most topic areas because of a paucity of methodologically sound studies in the literature. These investigators stated that more rigorously designed studies are needed to examine outcomes of interest, with fewer sources of potential error or bias. Level of Evidence = V.
The guideline provided the following recommendations:
- The workgroup suggests that surgeons perform concurrent upper eyelid blepharoplasty and ptosis correction in patients presenting with ptosis and dermatochalasis (excess upper eyelid soft tissue hooding). (Low level of evidence; weak recommendation)
- The workgroup suggests that surgeons perform upper eyelid blepharoplasty in patients presenting with dermatochalasis without underlying ptosis. (Low level of evidence; weak recommendation)
- It is an option for surgeons to perform adjunctive brow surgery in patients presenting with dermatochalasis and co-existing brow and upper eyelid ptosis. (Low level of evidence; option)
- It is an option for surgeons to perform levator plication or levator advancement for patients presenting with upper eyelid ptosis. (Very low level of evidence; option)
Glossary of Terms
| Term | Definition |
|---|---|
| Blepharoplasty | Surgical repair or reconstruction of the eyelid |
| Brow ptosis | Drooping of the eyebrow |
| Corneal light reflex | Reflection of light off of the corneas |
| Ectropion | Eyelid turned outward |
| Entropion | Eyelid turned inward |
| Margin to reflex difference | Distance between the upper eyelid margin and the corneal light reflex |
| Ptosis surgery | Surgery to tighten the muscles of the drooping eyelid or eyebrow |
| Superior visual field | Upper half of visual field |
| Upper lid ptosis | Drooping of the upper eyelid |
| Visual field | Area that a person is able to see with fixed gaze |
References
The above policy is based on the following references:
- Adamson PA, Strecker HD. Transcutaneous lower blepharoplasty. Facial Plast Surg. 1996;12(2):171-183.
- Al-Abbadi Z, Sagili S, Malhotra R. Outcomes of posterior-approach 'levatorpexy' in congenital ptosis repair. Br J Ophthalmol. 2014;98(12):1686-1690.
- Alfano C, Chiummariello S, De Gado F, et al. Lateral canthoplasty -- 10-year experience. Acta Chir Plast. 2006;48(3):85-88.
- American Academy of Ophthalmology. Functional indications for upper and lower eyelid blepharoplasty. Ophthalmology. 1995;102(4):693-695.
- American Academy of Ophthalmology. Laser blepharoplasty and skin resurfacing. Ophthalmology. 1998;105(11):2154-2159.
- American Optometric Association. Care of the patient with amblyopia. Optometric Clinical Practice Guideline No. 4. 2nd ed. St. Louis, MO: American Optometric Association; 1997.
- American Society of Plastic and Reconstructive Surgeons. Blepharoplasty Position Paper. Arlington Heights, IL: American Society of Plastic and Reconstructive Surgeons, Inc.; October 1990.
- American Society of Plastic Surgeons. Blepharoplasty. ASPS recommended insurance coverage criteria for third-party payers. Arlington Heights, IL: American Society of Plastic Surgeons; 2007.
- American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS). 2015. White Paper on Functional Blepharoplasty, Blepharoptosis, and Brow Ptosis Repair. Available at: https://www.asoprs.org/assets/docs/1%20-%20FINAL%20ASOPRS%20White%20Paper%20January%202015.pdf. Accessed March 17, 2023.
- An SH, Jin SW, Kwon YH, et al. Effects of upper lid blepharoplasty on visual quality in patients with lash ptosis and dermatochalasis. Int J Ophthalmol. 2016;9(9):1320-1324.
- Antus Z, Salam A, Horvath E, Malhotra R. Outcomes for severe aponeurotic ptosis using posterior approach white-line advancement ptosis surgery. Eye (Lond). 2018;32(1):81-86.
- Apfelberg DB. Summary of the 1997 ASAPS/ASPRS Laser Task Force Survey on laser resurfacing and laser blepharoplasty. American Society for Aesthetic Plastic Surgery. American Society of Plastic and Reconstructive Surgeons. Plast Reconstr Surg. 1998;101(2):511-518.
- Barnes JA, Bunce C, Olver JM. Simple effective surgery for involutional entropion suitable for the general ophthalmologist. Ophthalmology. 2006;113(1):92-96.
- Baylis HI, Goldberg RA, Kerivan KM, et al. Blepharoplasty and periorbital surgery. Dermatol Clin. 1997;15(4):635-647.
- Bedran EG, Pereira MV, Bernardes TF. Ectropion. Semin Ophthalmol. 2010;25(3):59-65.
- Benatar M, Kaminski H. Medical and surgical treatment for ocular myasthenia. Cochrane Database Syst Rev. 2006;(2):CD005081.
- Biesman BS. Blepharoplasty. Semin Cutan Med Surg. 1999;18(2):129-138.
- Broujerdi JA. Aesthetic surgery of the orbits and eyelids. Oral Maxillofac Surg Clin North Am. 2012;24(4):665-695.
- Burnstine MA, Putterman AM. Upper blepharoplasty: A novel approach to improving progressive myopathic blepharoptosis. Ophthalmology. 1999;106(11):2098-2100.
- Cahill KV, Bradley EA, Meyer DR, et al. Functional indications for upper eyelid ptosis and blepharoplasty surgery: A report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(12):2510-2517.
- Centers for Medicare & Medicare Services (CMS). Local Coverage Article: Blepharoplasty - Medical Policy Article (A52837). Baltimore, MD: CMS; effective January 1, 2018.
- CGS Administrators, LLC. Local coverage determination (LCD): Blepharoplasty. LCD ID L33944. Medicare Administrative Contractor (MAC) Part A/B. Nashville, TN: CGS Administrators; revised October 1, 2015.
- Chang S, Lehrman C, Itani K, Rohrich RJ. A systematic review of comparison of upper eyelid involutional ptosis repair techniques: Efficacy and complication rates. Plast Reconstr Surg. 2012;129(1):149-157.
- Dailey RA, Saulny SM. Current treatments for brow ptosis. Curr Opin Ophthalmol. 2003;14(5):260-266.
- Davies RP. Surgical options for eyelid problems. Aust Fam Physician. 2002;31(3):239-245.
- de Figueiredo AR. Blepharoptosis. Semin Ophthalmol. 2010;25(3):39-51.
- Edmonson BC, Wulc AE. Ptosis evaluation and management. Otolaryngol Clin North Am. 2005;38(5):921-946.
- Fedok FG, Perkins SW. Transconjunctival blepharoplasty. Facial Plast Surg. 1996;12(2):185-195.
- Fong KC, Mavrikakis I, Sagili S, Malhotra R. Correction of involutional lower eyelid medial ectropion with transconjunctival approach retractor plication and lateral tarsal strip. Acta Ophthalmol Scand. 2006;84(2):246-249.
- Friedland JA, Jacobsen WM, TerKonda S. Safety and efficacy of combined upper blepharoplasties and open coronal browlift: A consecutive series of 600 patients. Aesthetic Plast Surg. 1996;20(6):453-462.
- Frueh BR, Musch DC, McDonald HM. Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology. 2004;111(12):2158-2163.
- Gundisch O, Vega A, Pfeiffer MJ, Hintschich C. The significance of intraoperative measurements in acquired ptosis surgery. Orbit. 2008;27(1):13-18.
- Hahn S, Holds JB, Couch SM. Upper lid blepharoplasty. Facial Plast Surg Clin North Am. 2016;24(2):119-127.
- Hashem AM, Couto RA, Waltzman JT, et al. Evidence-based medicine: A graded approach to lower lid blepharoplasty. Plast Reconstr Surg. 2017;139(1):139e-150e.
- Hatt S, Antonio-Santos A, Powell C, Vedula SS. Interventions for stimulus deprivation amblyopia. Cochrane Database Syst Rev. 2006:(3):CD005136.
- Ho SF, Pherwani A, Elsherbiny SM, Reuser T. Lateral tarsal strip and quickert sutures for lower eyelid entropion. Ophthal Plast Reconstr Surg. 2005;21(5):345-348.
- Hollander MHJ, Contini M, Pott JW, et al. Functional outcomes of upper eyelid blepharoplasty: A systematic review. J Plast Reconstr Aesthet Surg. 2019;72(2):294-309.
- Hollander MHJ, Schortinghuis J, Vissink A, et al. Aesthetic outcomes of upper eyelid blepharoplasty: A systematic review. Int J Oral Maxillofac Surg. 2020;49(6):750-764.
- Hong SP, Song SY, Cho IC. Under-through levator complex plication for correction of mild to moderate congenital ptosis. Ophthal Plast Reconstr Surg. 2014;30(6):468-472.
- Ing E. Ectropion treatment & management. Medscape. New York, NY: WebMD: updated: July 20, 2018. Available at: https://emedicine.medscape.com/article/1212398-treatment. Accessed September 10, 2018.
- Januszkiewicz JS, Nahai F. Transconjunctival upper blepharoplasty. Plast Reconstr Surg. 1999;103(3):1015-1019.
- Kikkawa DO, Kim JW. Lower-eyelid blepharoplasty. Int Ophthalmol Clin. 1997;37(3):163-178.
- Kikkawa DO, Miller SR, Batra MK, et al. Small incision nonendoscopic browlift. Ophthal Plast Reconstr Surg. 2000;16(1):28-33.
- Kim KK, Granick MS, Baum GA, et al. American Society of Plastic Surgeons evidence-based clinical practice guideline: Eyelid surgery for upper visual field improvement. Plast Reconstr Surg. 2022;150(2):419e-434e.
- King M. Management of ptosis. J Clin Aesthet Dermatol. 2016;9(12):E1-E4.
- Kumar S, Kamal S, Kohli V. Levator plication versus resection in congenital ptosis - a prospective comparative study. Orbit. 2010;29(1):29-34.
- Lee JH, Aryasit O, Kim YD, et al. Maximal levator resection in unilateral congenital ptosis with poor levator function. Br J Ophthalmol. 2017;101(6):740-746.
- Lee MS. Overview of ptosis. UpToDate [online serial]. Waltham, MA: UpToDate; reviewed October 2013.
- Lessner AM, Fagien S. Laser blepharoplasty. Semin Ophthalmol. 1998;13(3):90-102.
- Mahe E. Lower lid blepharoplasty-The transconjunctival approach: Extended indications. Aesthetic Plast Surg. 1998;22(1):1-8.
- Meyer DR, Linberg JV, Powell SR, Odom JV. Quantitating the superior visual field loss associated with ptosis. Arch Ophthalmol. 1989;107(6):840-843.
- National Government Services, Inc. Local coverage article: Blepharoplasty. Article ID A52837. Medicare Administrative Contractor (MAC) Part A/B. East Syracuse, NY: National Government Services; revised January 1, 2018.
- Older JJ. Ptosis repair and blepharoplasty in the adult. Ophthalmic Surg. 1995;26(4):304-308.
- Pacella E, Mipatrini D, Pacella F, et al. Suspensory materials for surgery of blepharoptosis: A systematic review of observational studies. PLoS One. 2016;11(9):e0160827.
- Pastorek N. Upper-lid blepharoplasty. Facial Plast Surg. 1996;12(2):157-169.
- Rosenberg JB, Andersen J, Barmettler A. Types of materials for frontalis sling surgery for congenital ptosis. Cochrane Database Syst Rev. 2019;4:CD012725.
- Rougraff PM, Tse DT, Johnson TE, Feuer W. Involutional entropion repair with fornix sutures and lateral tarsal strip procedure. Ophthal Plast Reconstr Surg. 2001;17(4):281-287.
- Sakol PJ, Mannor G, Massaro BM. Congenital and acquired blepharoptosis. Curr Opin Ophthalmol. 1999;10(5):335-339.
- Schaefer DP. The graded levator hinge procedure for the correction of upper eyelid retraction (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007;105:481-512.
- Scuderi N, Chiummariello S, De Gado F, et al. Surgical correction of blepharoptosis using the levator aponeurosis-Müller's muscle complex readaptation technique: A 15-year experience. Plast Reconstr Surg. 2008;121(1):71-78.
- Shields M, Putterman A. Blepharoptosis correction. Curr Opin Otolaryngol Head Neck Surg. 2003;11(4):261-266.
- SooHoo JR, Davies BW, Allard FD, Durairaj VD. Congenital ptosis. Surv Ophthalmol. 2014;59(5):483-492.
- Stephenson CB. Upper-eyelid blepharoplasty. Int Ophthalmol Clin. 1997;37(3):123-132.
- Uslu A. Use of a perforator/subcutaneous pedicled propeller flap for reconstruction of lower eyelid defects. J Plast Reconstr Aesthet Surg. 2019;72(1):119-124.
- Yang X, Jin Y, Lin X, et al. Management of periorbital microcystic lymphatic malformation with blepharoptosis: Surgical treatment combined with intralesional bleomycin injection. J Pediatr Surg. 2015;50(8):1393-1397.

