Los enlaces a los sitios que no son de Aetna se brindan únicamente para su comodidad. Aetna Inc. y sus compañías afiliadas no son responsables del contenido, la precisión o las prácticas de privacidad de los sitios vinculados, ni de los productos o servicios descritos en dichos sitios.
Now it’s personal: How data and analytics are humanizing health care
 Por Maureen Shelly
Por Maureen Shelly

You might imagine that when you experience a health crisis, your doctor carefully considers your medical history, family history and lifestyle when weighing diagnoses and treatments. In fact, aside from high-level considerations like age and gender, that’s often not the case. Traditionally, diagnoses are one-size-fits-all, and optimal treatments are determined through trial and error. In medicine’s early days, that was the best we could do. If you had cancer, the location of the growth would determine your treatment. Then we discovered that cancer comes in different genetic subtypes, with distinct progressions and treatment protocols. Today, doctors no longer treat all cancers the same.
Medicine is beginning to acknowledge that not all patients are the same either. The biological, psychological and social factors that led to your disease are not those of the person next to you in the waiting room. And those factors impact how you’ll respond to treatment and your risk of complications.
Personalized medicine refers to the customization of medical decisions to the individual patient, based on their DNA, medical history, family history, environment, behavior, culture and values. The goal is to find the most effective approach for a particular patient ― which is often the most cost-efficient approach as well.
We all know that U.S. health care spending is out of control. America spends two to three times more than most developed countries, and with worse results. The Centers for Disease Control and Prevention (CDC) estimates that 90% of the nation’s health spending goes to chronic and mental health conditions.1 Prevention and proper management can greatly reduce these costs.
In this article, we’ll explore how personalization is lowering health spending through a focus on early intervention. We’ll examine the data inputs and analytic tools making those interventions possible. And we’ll show that, while traditional care dehumanizes, personalization rehumanizes, resulting in a better patient experience.
The Angelina Jolie effect: What you need to know about genetic testing
In 2013, Angelina Jolie famously revealed she’d undergone a preventive double mastectomy after testing positive for the BRCA1 gene variant. Her story spurred a dramatic increase in genetic health tests. In the 15 days after her essay appeared in The New York Times, testing for BRCA1 and BRCA2 spiked 64%, translating to an extra 4,500 tests among U.S. women.2 DNA health testing had gone mainstream.

Genetic screening for use in health risk assessment, diagnosis and treatment is sometimes referred to as “precision medicine.” Since 1998, Aetna has been a key player in developing best practices around genetic testing, while advocating for wider access to genetic services, protecting patient privacy and promoting nondiscrimination policies.
“One of the most important jobs a health plan can perform is to make sure our members have access to the tests that have a clinical benefit,” says Heather Shappell, a board-certified genetic counselor who manages Aetna’s Precision Medicine program. “There are tests that might be available ― and even marketed pretty extensively ― that really don’t have any proven value.” Aetna covers thousands of genetic tests for its members.
Experts usually recommend genetic testing only when a patient has a specific medical reason, such as a family history of certain cancers. Genetic counselors, like those promoted by Aetna, can steer patients toward the high-quality tests that are appropriate for them, and thoroughly explain how the results might shape future health decisions.
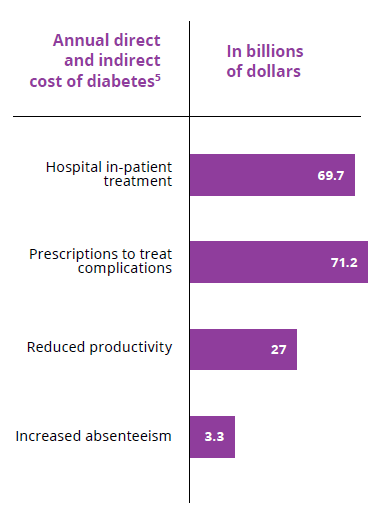
Aunque la cobertura mediática tiende a centrarse en el papel de la genética en el diagnóstico y el tratamiento del cáncer, las pruebas de ADN pueden medir miles de riesgos distintos para la salud. En octubre del 2018, por ejemplo, la Asociación Americana de la Diabetes (ADA) publicó un estudio sobre la promesa de la medicina de precisión en la prevención y el tratamiento de la diabetes de tipo 2, la enfermedad más cara en Estados Unidos. Aproximadamente la mitad de las personas con diabetes tipo 2 tienen una predisposición genética, lo que indica que hay subtipos con diferente progresión y riesgo de tener, por ejemplo, enfermedad renal y enfermedad de la arteria coronaria. En 2017, la diabetes costó a los estadounidenses unos $237,000 millones en costos médicos directos4. La intervención temprana tiene el potencial de ahorrar más de $100,000 millones.
Although the use of genomics in diabetes treatment is some years off, the study’s authors predict a rapid evolution of new treatment regimens that “are more effective, less costly, and convey fewer unnecessary side effects.” Aetna’s comprehensive approach to precision medicine positions us to take advantage of new genetic technologies and services while controlling medical costs.
As you can see, personalization shifts health care’s focus upstream, from reactive crisis management to prediction and prevention. In this way, the approach is more aligned with patient values. After all, we tend to see our doctor for symptoms that affect our quality of life. The future of health care will be about extending not just our lifespan, but our healthspan: the years when we are in generally good health and able to enjoy life on our terms.
Read more about how precision medicine improves the patient experience:
- 6 things to know before you get a genetic health test.
- Patient story: A mother and daughter fight breast cancer together.

The art of the nudge: Wearable tech helps drive behavior change
Like genetic testing, wearable devices introduce a whole new data stream to medical decision making. Wearables can provide doctors with real-time information on activity levels (exercise, sleep patterns) and vital signs (heart rate, blood pressure, breathing, blood-sugar levels) that allow for early detection of problems and personalized interventions. Some devices even nudge users to take healthy actions, like going for a brief walk if they’ve been sedentary too long, or de-stressing with a mindful moment.
En enero del 2019, Aetna anunció la aplicación Attain by Aetna℠ en colaboración con Apple®. Se trata de una herramienta de salud única en su clase, que combina los registros de salud de los miembros con la actividad de su Apple Watch® para ofrecer objetivos personalizados y que se puedan alcanzar. Las recomendaciones van mucho más allá del bienestar físico y se centran en las medidas que mejoran los resultados de salud y la productividad, y reducen los costos: Se les puede recomendar a los usuarios vacunarse contra la influenza, renovar una receta o cambiar a un laboratorio dentro de la red. Cuando cumplen con lo previsto, se los recompensa con tarjetas de regalo de las principales tiendas al por menor. Pero las empresas serán las que disfruten de verdaderas recompensas: La influenza costó a los empleadores estadounidenses aproximadamente $21,000 millones en pérdida de productividad durante la temporada de la influenza del 2017 y 20186.
Wearables tap into many of the psychological techniques that keep us reaching for our phones. Gamification and social competition can be powerful motivators that maintain member engagement over the long term. Wearables also enable health care systems to gather anonymized data in order to predict trends and test appropriate interventions (more on that below).
Más información sobre la aplicación Attain by Aetna
Apple, el logotipo de Apple logo, Apple Watch y iPhone son marcas comerciales de Apple, Inc., registradas en los Estados Unidos y en otros países.
What's blockchain got to do with it: The benefits of electronic medical records
In theory, your entire medical history should live in the cloud, accessible by any health provider who needs to reference or add to it. In reality, each doctor or facility you visit has part of your medical record, but very few have access to all of it, due in large part to incompatible platforms.
Esta fragmentación de los registros de los pacientes produce malgasto y errores médicos. En 2012, la Academia Nacional de Medicina estimó que el malgasto representa el 25 % de todo el gasto de salud de Estados Unidos cada año, es decir $765,000 millones7. Los médicos suelen pedir una segunda prueba porque no pueden ver los resultados de los análisis solicitados por otros consultorios. Peor aún, a los pacientes que consultan a varios médicos se les pueden recetar medicamentos que interactúan negativamente entre sí, lo que provoca efectos secundarios graves y retrasos en el tratamiento.
Hasta ahora, los distintos registros de los pacientes no se pudieron reunir en una única historia. La respuesta puede estar en el mundo de las criptomonedas. Blockchain es una tecnología que da sentido a la información descentralizada manteniendo la seguridad. Luego de demostrar que es capaz de proteger a los propietarios de bitcoins, la tecnología blockchain está preparada para ahorrarle a Estados Unidos $7.9 mil millones en pruebas duplicadas de laboratorio y radiología debido a la falta de datos compartidos8.
In early 2019, IBM announced a collaboration with Aetna and other companies to test out a version of blockchain called Hyperledger Fabric. The system will work to collect, streamline and standardize medical record keeping. “Blockchain has the potential to produce an information ecosystem that finally connects all of the health players,” says Claus Jensen, chief technology officer for CVS Health and Aetna. “My ambition is to position CVS Health as an information hub for the health sector as a whole.”
By allowing for easy data sharing between providers, blockchain should reduce inefficiencies and errors. It could also address other health system challenges, from processing claims and payments to maintaining accurate provider directories. “The greatest promise of blockchain,” says Jay Rajda, MD, Aetna’s senior medical director of medical affairs, “is the ability to make more complete information available in a more timely fashion, at the point of decision making. Better information leads to better clinical care. And you’re going to improve the consumer experience tremendously.”
The AI advantage: Transforming data into actionable insights
Personal data is merely raw material. Artificial intelligence (AI) is the computer brain that spins it into valuable insight. Studies show that pattern recognition programs can help diagnose disease with greater speed and accuracy than humans alone. Algorithms are beginning to point doctors to the best treatment protocols. Most significantly, predictive analytics are flagging which individuals are at the highest risk for developing serious conditions ― once again, shifting the focus of health care upstream to prevention.
Launched in 2018, Aetna’s Next Best Action initiative encourages individuals to take one small step at a time toward achieving a healthier life. The term next best action refers to the use of a customer’s data (past behavior, preferences, etc) to guide him or her toward certain decisions or services. Digital companies like Amazon and Netflix have been doing this for years with their product-recommendation engines. In health care, the simpler and more specific each ask is, the more likely the member is to complete the action.
A continuación verá cómo un programa de Aetna utiliza los registros de salud y el análisis de datos para resolver problemas que se dan en el mundo real de una miembro ficticia llamada Greta. El objetivo es la intervención temprana, que mantiene a las personas más saludables y, al mismo tiempo, reduce los costos médicos. La iniciativa Next Best Action aprovecha una oportunidad de margen de más de $250 millones, incluso cuando se dirige a una pequeña fracción de la población completamente asegurada de Aetna.
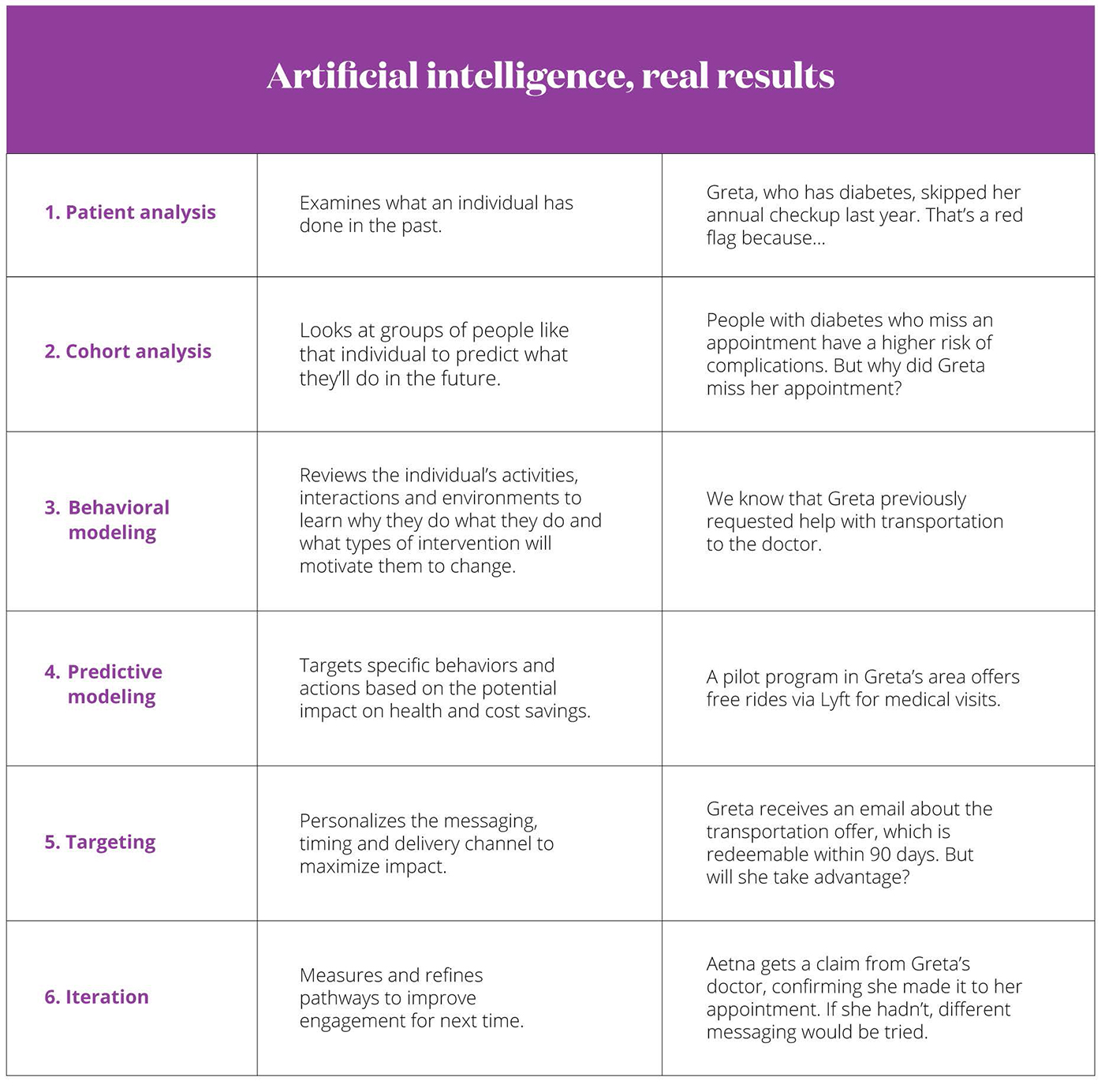
Customer service is another area where AI can create a more personalized experience. The Aetna Concierge program gives call-in centers enhanced data to address callers’ needs quickly and easily. For instance, if a caller is looking for information on virtual care, the rep is alerted that the caller has children. The rep then knows to inform the caller that the Teladoc service provides access to board certified pediatricians. Because member needs shift over time, the algorithm reevaluates what’s important to individuals every month.

The benefits to health and the bottom line
Está demostrado que una personalización eficaz reduce los efectos secundarios adversos y las internaciones. Dado que el 90 % del gasto de salud se destina a enfermedades crónicas, el posible ahorro económico es asombroso. Solo prevenir las complicaciones de la diabetes podría ahorrar a los estadounidenses más de $100,000 millones cada año. Y dado que $765,000 millones se desperdician anualmente, reducir la duplicación de pruebas y otras ineficiencias podría ahorrar muchos miles de millones más.
Cost savings aside, personalization aligns success more closely with patient values and health goals, making individuals feel recognized and understood. That results in better patient participation, compliance and satisfaction. By treating each patient as a unique person rather than a broad diagnostic label, we can rehumanize the health care system.
“I see more and more algorithmic work being taken off the primary care doctor's plate, so that they can spend more time with the patients who need them the most,” says Troyen Brennan, MD, chief medical officer of CVS and Aetna. “Diabetes, high blood pressure, high cholesterol, depression, asthma — all lend themselves to a personalized approach that is more efficient and less expensive.”
To learn more about how your organization can benefit from Aetna’s personalized offerings, contact us
Footnotes:
2 Aetna International, “Bespoke health promotion: How personalization is transforming health”. 2018
3 American Diabetes Association, “A global overview of precision medicine in type 2 diabetes”. 2018
4 Asociación Americana de la Diabetes, “The cost of diabetes”. 2023
5 Challenger, Gray & Christmas, Inc. 2018
6 National Academy of Medicine, “Roundtable on value & science-driven healthcare”. 2012
7 “Value of information sharing in reducing health care waste”. 2014
Special thanks to:
Caroline Pain, Brian O’Gilvie and Lorien Norden at Aetna International for their original research.
Sobre la autora
Maureen Shelly es una aficionada a la salud y la ciencia que vive en la ciudad de Nueva York.
Share this whitepaper:
Now it's personal: How data and analytics are humanizing health care.
Now it's personal: How data and analytics are humanizing health care.